June 2024
Flat Feet
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.
Causes and Symptoms of Flat Feet
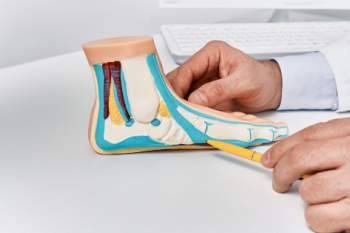
Flat feet, or fallen arches, occur when the arches of the feet do not develop properly or collapse over time. This condition can be caused by genetic factors, injury, arthritis, or the natural aging process. Obesity and pregnancy may also contribute to the development of flat feet due to increased pressure on the arches. Common symptoms include foot pain, particularly in the heel or arch area, swelling along the inside of the ankle, and difficulty standing on tiptoe. Flat feet can lead to problems with walking or running and may cause discomfort in the legs and lower back. Proper diagnosis and treatment by a podiatrist can help to manage symptoms and prevent further complications. If you have flat feet, it is suggested that you are under the care of this type of doctor who can help you manage this condition and guide you toward relief solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Managing Toenail Fungus Infections

Fungal toenail infections, or onychomycosis, account for approximately 50 percent of all nail diseases, particularly affecting toenails. Laboratory diagnosis through microscopy and culture of nail clippings is recommended before starting treatment to confirm the infection type. For patients requiring treatment of fungal toenails, oral antifungal medications are typically used for severe infections, while topical antifungals are suitable for superficial or minor cases and for those unable to take oral medications. The duration of treatment varies, with systemic medications typically requiring a few months and topical treatments possibly extending up to two years. Patients should be aware that treatment success rates vary, and nails may not return to a completely normal appearance even after successful therapy. Additionally, there is a risk of treatment failure or relapse, necessitating further diagnosis and possibly alternative treatment strategies. Ultimately, the decision to treat fungal nails should be individualized, considering the patient's overall health, risk factors such as diabetes or vascular disease, and the severity of the infection. If you have developed a fungal toenail infection, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment suggestions.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Dr. Kirk Sherris of Liberty Bay Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Arthritis and the Feet
 Arthritis can significantly impact the feet, leading to pain, swelling, and difficulty in walking. Several types of arthritis can affect the feet, with osteoarthritis and rheumatoid arthritis being the most common. Osteoarthritis, often referred to as wear-and-tear arthritis, occurs when the protective cartilage that cushions the ends of bones wears down over time. This can lead to pain and stiffness in the feet, particularly in the joints of the toes and ankles. Rheumatoid arthritis, on the other hand, is an autoimmune condition where the body's immune system attacks the joints, causing inflammation and deformity. Treatment options for arthritis in the feet vary depending on the type and severity of the condition. They may include medication to reduce pain and inflammation, exercise to improve joint function and mobility, and orthotic devices to support the feet. In severe cases, surgery may be necessary to repair or replace damaged joints. If you are experiencing foot pain or discomfort due to arthritis, it is suggested that you schedule an appointment with a podiatrist who can provide specialized care and a tailored treatment plan to alleviate the symptoms, and improve your quality of life.
Arthritis can significantly impact the feet, leading to pain, swelling, and difficulty in walking. Several types of arthritis can affect the feet, with osteoarthritis and rheumatoid arthritis being the most common. Osteoarthritis, often referred to as wear-and-tear arthritis, occurs when the protective cartilage that cushions the ends of bones wears down over time. This can lead to pain and stiffness in the feet, particularly in the joints of the toes and ankles. Rheumatoid arthritis, on the other hand, is an autoimmune condition where the body's immune system attacks the joints, causing inflammation and deformity. Treatment options for arthritis in the feet vary depending on the type and severity of the condition. They may include medication to reduce pain and inflammation, exercise to improve joint function and mobility, and orthotic devices to support the feet. In severe cases, surgery may be necessary to repair or replace damaged joints. If you are experiencing foot pain or discomfort due to arthritis, it is suggested that you schedule an appointment with a podiatrist who can provide specialized care and a tailored treatment plan to alleviate the symptoms, and improve your quality of life.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Are You Suffering From Ingrown Toenails?
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
Podiatrists Are Foot Health Specialists

A podiatrist, also known as a foot doctor, is a medical professional who specializes in diagnosing and treating conditions related to the feet, ankles, and lower extremities. Their primary focus is to ensure optimal foot health, addressing issues ranging from common ailments like bunions and ingrown toenails to complex conditions such as diabetic foot ulcers or sports injuries. In their workplace, podiatrists typically operate in clinics, hospitals, or private practices, equipped with diagnostic tools like X-rays and ultrasound machines. Podiatrists undergo extensive training, earning a Doctor of Podiatric Medicine, or DPM, degree from accredited podiatric medical schools. Some may further specialize in areas like sports medicine, wound care, or pediatric podiatry through postgraduate residencies or fellowships, honing their expertise to address specific patient needs effectively. If you are experiencing any type of foot condition, it is suggested that you consult a podiatrist who can offer you effective treatment solutions, in addition to answering any questions you may have about this field of medicine.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.